Spinal or back pain can occur anywhere along the backbone or vertebral column.
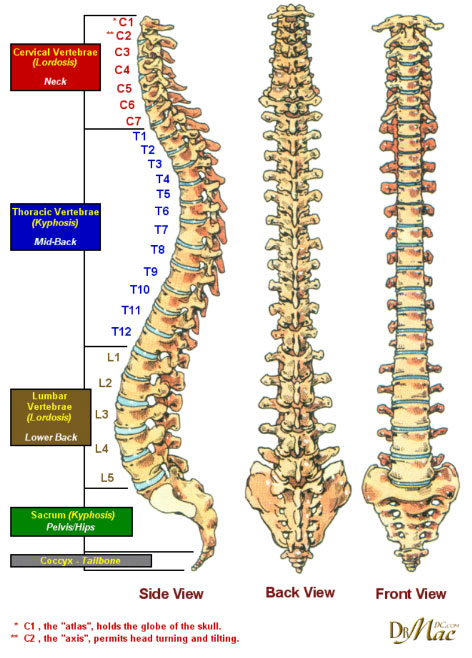
The vertebral column consists of five regions that start at the base of the skull and continue to the tail bone. These regions are called cervical (neck), thoracic (upper back from shoulders to the base of the rib cage), lumbar (midback to the top of the hip bone) and sacral (the back wall of the pelvis), and the coccygeus or tail bone. There are 7, 12, 5, 5, and 3-5 of each type of vertebra, respectively. The sacrum and coccygeus are fused.
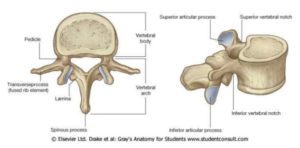
Each vertebral segment contains one vertebral body, 2 pedicles, 2 laminas, 2 transverse processes, 2 superior and inferior articular processes, and one spinous process. The opening between the body and the arch is the spinal canal and is where the spinal cord travels from the brain to the sacrum. The spinous process is the part of the spine that one can see and feel in the back.
Ligaments run up and down the vertebra and side to side while the intervertebral discs are in between each vertebra and act to cushion the joints and allow for movement such as bending and twisting. They are composed fibrous and jelly-like substances. The nerve roots come out of the spinal cord in between the vertebra and send out smaller nerves to all parts of the body. There are muscles around the spinal column and blood vessels to supply all regions of the spine and spinal cord.
The following risk factors have been associated with the development of spinal pain:
- Jobs that are stressful and that require heavy lifting and use of heavy equipment
- Trauma, falls, car accidents
- Cigarette smoking
- Psychiatric, emotional, and personality issues
- Obesity
- Spinal deformities and endplate injury
- Genetic predisposition
- Peripheral vascular disease
- Osteoporosis
VINDICATE
In general, there are nine general categories of conditions or diseases that can affect the vertebra, the spinal cord, ligaments, nerves, joints, muscles, and blood vessels. VINDICATE is a useful mnemonic to remember the potential causes for any disease or injury to the spine. Collectively, any of these conditions can lead to pain, paralysis, numbness, burning, tingling, immobility, and gait disturbances.
- V – Vascular
- I – Inflammatory
- N – Neoplastic-cancer
- D – Degenerative / Deficiency
- I – Idiopathic (unknown), Intoxication
- C – Congenital or genetic
- A – Autoimmune / Allergic-Rheumatoid arthritis
- T – Traumatic
- E – Endocrine-osteoporosis
Lumbar / Low Back Pain
Almost 30% of the patients with acute onset low back pain (LBP) will progress to develop chronic LBP that is typically unresponsive to available treatments. People with back pain who were off work for 6 months with LBP had lifetime return to work rate of only 50%; this rate further dropped to 25% for workers who were off work for 1 year, and to less than 5% for those who were off work for 2 years. The lifetime incidence of LBP is therefore reported variably, ranging from 14% to as high as 90%. Acute LBP has been ranked as the fifth most common reason for all physician visits; in a given year almost 50% of adults will have LBP.
Most Common Causes of Lumbar Back Pain are:
- Disc Degeneration
- Disc Herniation
- Lumbar Stenosis
- Lumbar Strain or Sprain
- Spondylolisthesis
- Vertebral Compression Fracture
Lumbar (low back) degenerative disc disease (DDD) is a common in aging adults. The intervertebral discs gradually dry out, losing strength and resiliency. In most people, these changes are gradual. If the disc’s outer wall cracks or breaks open, the gel inside the disc can leak out causing a herniated disc. The disc material may place pressure on nearby nerve roots or the spinal cord. Additionally, disc material releases chemical irritants causing nerve inflammation and pain.
Symptoms
DDD can cause discs to lose height and become stiff. When disc height is lost, nerve impingement, bone and joint inflammation, and pain can occur. Disc degeneration causes loss of the joint space, similar to arthritis pain and inflammation. In severe cases, pain may be constant.
Symptoms of Herniated Disc
- Dull or sharp low back pain intensified by bending, coughing, sneezing, or other movement
- Muscle spasm or cramping
- Sciatica (pain, burning, tingling, and numbness that extends from the buttock into the leg or foot)
- Leg weakness or loss of leg function
There are four stages of herniation: disc degeneration, protrusion, extrusion, and sequestration, which is stage 4 where the contents completely breakthrough and leak out of the wall
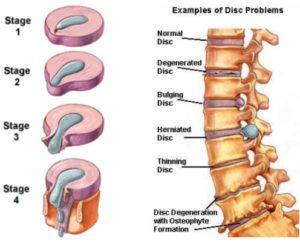
Basically, any disc can undergo these changes including the thoracic (chest) and cervical (neck) regions.
Lumbar Stenosis
Lumbar spinal stenosis develops when either the spinal canal or nerve passageways (opening or foramen) become narrow. Lumbar central stenosis occurs if the spinal canal is narrowed. If the foramen is narrowed, it is called lumbar foraminal stenosis. In both cases, the spinal cord and/or nerves are compressed. Sometimes, patients have both types of lumbar stenosis.
Some patients are born with this narrowing (congenital). However, most cases of lumbar stenosis develop in patients over age 50 and results from aging and wear and tear on the spine. Other common causes include osteoarthritis, degenerative disc disease, or bone spurs (osteophytes).
A common cause of a sprain or strain is excessive physical demand on the spine’s ligaments or muscles. Although pain can be severe, and even temporarily disabling, most low back sprains and strains are easy to treat and do not require spine surgery.
Lumbar Strain or Sprain
A common cause of a sprain or strain is excessive physical demand on the spine’s ligaments or muscles. Although pain can be severe, and even temporarily disabling, most low back sprains and strains do not require spine surgery.
Sprains and strains are soft tissue injuries. Soft tissues include tendons, ligaments, and muscles. Sprains are limited to tendons and ligaments, whereas strains affect muscles. Injury can occur when these tissues are stretched beyond their normal limits.
Such as:
- Excessive flexion (bending forward)
- Excessive extension (bending backward)
- Excessive force to the spine (i.e. lifting or carrying a heavy object)
Spondylolisthesis
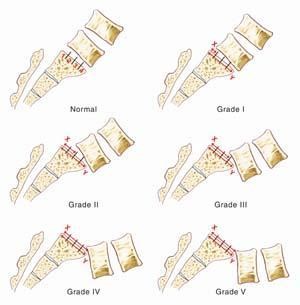
Spondylolisthesis is a spinal condition in which one vertebra slips forward over the vertebra below. Degenerative spondylolisthesis usually occurs in the lumbar (low back) spine, more commonly at L4-L5 or the 4th and 5th lumbar vertebral levels. Spondylolisthesis can result from degenerative changes in the vertebral structure that causes the vertebral joints to slip forward and may lead to spinal stenosis. Degenerative spondylolisthesis is most common among older female patients, usually over age 60.
Some people with spondylolisthesis are symptom-free and only find out when seeing their doctor for another health problem.
Symptoms may include:
- Low back pain
- Sciatica or muscle spasms
- Leg weakness
- Tight hamstring muscles
- Irregular gait or limp
Doctors use a Grading System to classify the degree of vertebral slippage. Slips are graded on the basis of the percentage that one vertebral body has slipped forward over the vertebral body below. Class 1 and II do not require surgery in general. Class III and IV are more likely to need surgery.
- Grade I: 1-24%
- Grade II: 25-49%
- Grade III: 50-74%
- Grade IV: 75%-99% slip.
- Grade V: Complete slip (100%), known as spondyloptosis
Vertebral Compression Fractures
A vertebral compression fracture occurs when a bony vertebral body collapses. This is often related to osteoporosis, a metabolic (endocrinologic) disease leading to loss of bone density (see right diagram below) that increases the risk of fracture. Osteoporosis can make a minor fall or simple bending and lifting movements traumatic. Compression fractures and other spinal fractures can also be caused by certain types of cancer or tumors, although this is not common.

Many people do not realize sudden and intense back pain may be a sign of a compression fracture. Whether painful or not, compression fractures can lead to additional fractures, spinal deformity, and loss of the ability to function.
Other signs and symptoms include:
- Loss if height (one of the reasons many older people seem to shrink as they age)
- Kyphosis (or humpback)
- Loss of balance (which increases the risk of falling)
- Neurological symptoms such as numbness, tingling, or weakness (which increases the risks of falling and subsequent fractures of other bones)